CULTURES OF WELLNESS
Self-Care as an Institutional Value
The prevailing ethos of putting the Triple Aim first at all costs - resulting in inordinate amounts of work is put on the backs of clinicians - simply cannot be maintained. But under the Hippocratic Oath, a lot of physicians feel compelled to comply in the "best interests of the patient". Is there another way? Have you considered the recently modified Geneva Oath and creating a culture where self-care is the expected norm of professionalism?
The Quadruple Aim was introduced by Drs. Thomas Bodenheimer and Christine Sinsky in a 2014 Annals in Family Medicine article to add the goal of improving the work life of health care providers, including physicians and staff.
The Quadruple Aim was introduced by Drs. Thomas Bodenheimer and Christine Sinsky in a 2014 Annals in Family Medicine article to add the goal of improving the work life of health care providers, including physicians and staff.
Redesigning Facility to Support Teamwork
Let's face it: our surroundings shape the way we interact with each other, whether it is at home, in a coffee shop or at medical practice. The way you interact with patients and colleagues can be subtly influenced by the design of your workspace. And even if you didn't get to design it from the ground up, there are subtle ways you can change things to make a difference.
Supporting Collegiality
Technology, industry pressure, and even the widespread use of hospitalists has deeply impacted physician relationships with each other. Recovering collaborative professional collegiality will be a huge key to the reduction of physician burnout.
Shame and the Culture of Medicine
It is well understood that shame is used as a pedagogical structure that is used to shape the behavior of future physicians. While some degree of shame is useful in societal structures to curb undesirable behavior, its weaponization in medical culture is legendary and destructive. The Shame Space is a project of Duke University to explore shame in healthcare through dialog.
Disruptive Physicians
While the phrase "disruptive physicians" can easily be thrown around or weaponized against doctors who simply want to see real change happen, there are times when doctors are actually affecting patient care and safety and team morale. Treating them fairly is a leadership skill that hospital and group practice employers need to get under their belt.
Code Lavender
This is a crisis intervention tool used to support any person in a Cleveland Clinic hospital. Patients, family members, volunteers, and healthcare staff can call a Code Lavender when a stressful event or series of stressful events occurs in the hospital. After the code is called, the Code Lavender team responds within 30 minutes.
Areas of Worklife SurveyIn 1999, the author of the Maslach Burnout Inventory and an organizational specialist, wrote a groundbreaking book helping employers understand the systems level causes of employee burnout, why they should do something about it, and how to intervene. Below is an overview of the six areas of worklife survey and contrasted with the MBI.
|
The Board of Medicine Application
Evidence shows that doctors nationwide are reluctant to seek help because of questions on the Board of Medicine's licensing application. In 2009, a study showed that up to 69% of state board applications included "likely impermissable" or "impermissable" items based on current Americans with Disabilities Act and case law. In Idaho, we have been successful in helping prod our state board along to eliminate application questions around mental health that delve further than current impairment. Additionally, if a physician is is current successful treatment for mental health concerns, this does not need to be reported on the new or renewal application. Fortunately, the Federation of State Boards of Medicine is moving on this issue and in 2018 made recommendations to state member boards that were very progressive and with intent to change the overall culture of medicine.
Here's the North Carolina story in Forbes Magazine of how they were successful in addressing this issue, as well as an earlier post on the Western Carolina Medical Society page.
Here's the North Carolina story in Forbes Magazine of how they were successful in addressing this issue, as well as an earlier post on the Western Carolina Medical Society page.
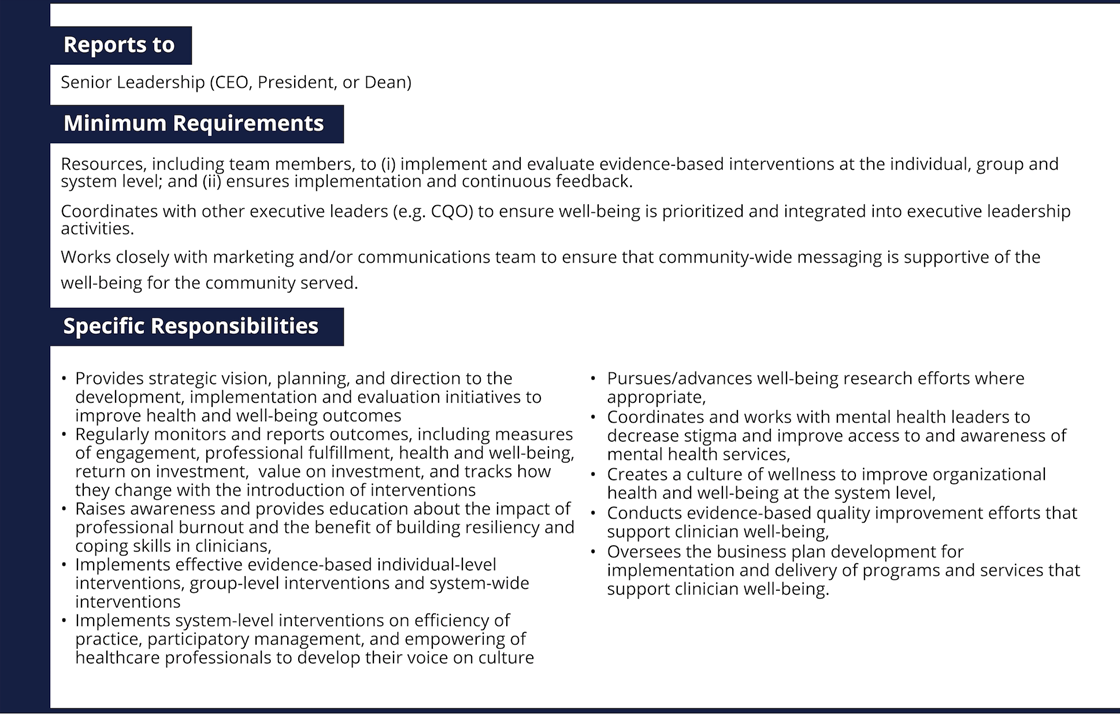
Chief Wellness Officer
|
In 2017, Dr. Tait Shanafelt, MD left Mayo Clinic and took the first known academic medical center Chief Wellness Officer role at Stanford Medicine. (Although, Barbara Hernandez should get some credit for playing a similar wellness role at Loma Linda University for many years, albeit not a physician and not a C-Suite leader.)
Since it was Dr. Shanafelt's 2014 Mayo Clinic Proceedings report on burnout that set the national medical community on fire about the topic, everybody looked to this move as a significant move and suddenly hospitals began investigating some sort of bird-dog role for wellness at their institutions. But is this just another attempt at a one-shot panacea that hospitals and executives can point to and say, "We've addressed burnout. Now back to the salt mines?" The key, according to many thought leaders on this topic, will be to how much authority this new position has and what resources will be given to them. Dr. Paul DeChant is a family physician, former CEO of Sutter Gould Health Foundation, and Deputy Chief Health Officer at Simpler Consulting, an IBM Watson Health company. He spends a lot of effort talking to C-Suite leaders about physician burnout and what their leadership can do to combat it through organizational efforts. According to DeChant, "A key to the role is having an effective way to impact and improve the clinical workplace, not simply support the worker. Therefore, reporting responsibility should be to the CEO, and decision authority should be on par with the COO, CFO, CMO, and CNO. In that way they can work as a team to address workplace dysfunction."
By the way, if you're thinking of creating a CWO role in your organization, consider anteing up $12K to go to Stanford's WellMD training they've started. It's a tidy sum, but if it prepares you to succeed at this new institutional challenge, you might end up saving your employer millions of dollars over the coming decade and your fellow physicians a whole lot of suffering. Sample CWO Job Description Source: “Making The Case For The Chief Wellness Officer In America’s Health Systems: A Call To Action, " Health Affairs Blog, October 26, 2018.DOI: 10.1377/hblog20181025.308059 |